PhD, RN
Evidence on: Skin-To-Skin After Cesarean
Originally published on August 8, 2012, and updated on October 25, 2023, by Sara Ailshire, MA, PhD Candidate, and Rebecca Dekker, PhD, RN.
To view our privacy policy, click here.
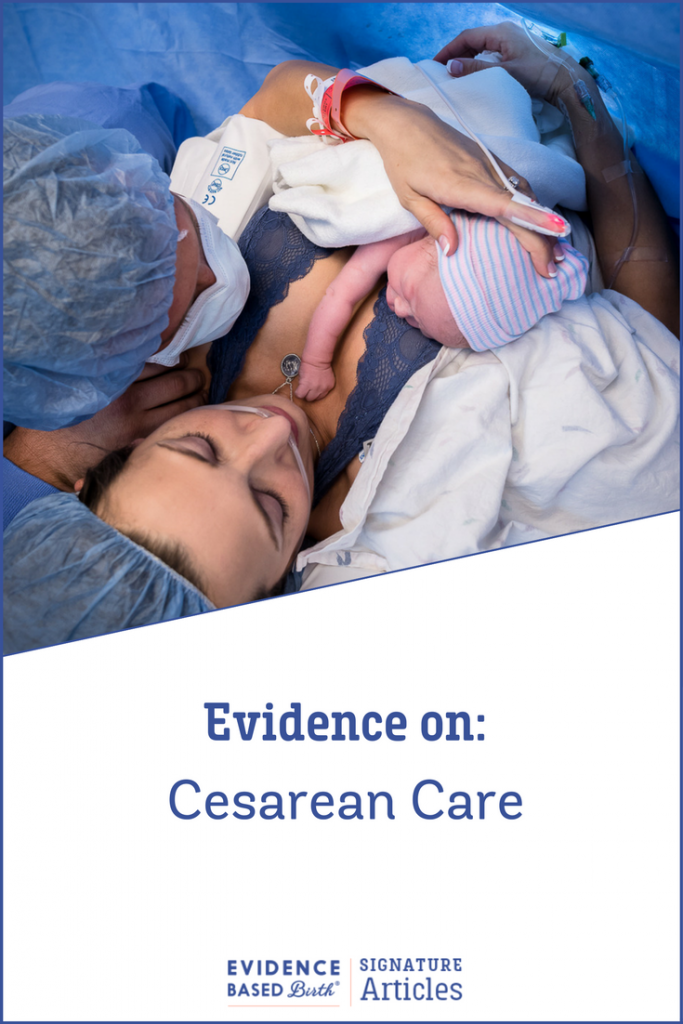
Skin-to-skin care (also called kangaroo care) is a natural process that involves placing a naked newborn on their parent’s bare chest and covering the infant with blankets to keep them dry and warm.
Ideally, skin-to-skin care starts immediately, or shortly, after birth, with the baby remaining on the parent’s chest until at least the end of the first nursing session (Moore et al. 2016). Note: Laying a baby on top of birthing parent’s gown or on top of a towel does not count as skin-toskin.
Skin-to-skin care can start at different times. In research, there are three main types of early skin- toskin care for healthy term infants:
- Birth or immediate skin-to-skin care starts during the first minute after birth.
- Very early skin-to-skin care begins within 30–40 minutes post-birth.
- Early skin-to-skin is any skin-to-skin time that takes place during the first 24 hours.
As we will describe in this article, skin-to-skin care after a Cesarean has many benefits for parents and babies. However, parents recovering from a Cesarean can’t do skin-to-skin if they are routinely separated from their babies. To do skin-to-skin, parents and newborns must be together.
Why aren’t babies kept with their parents after a Cesarean? Is it possible for hospitals to make the switch from routine separation to keeping families together, so that babies born by Cesarean can experience the benefits of skin-to-skin care? Keep reading to find out.
Lactation and Inclusive Language
Here at EBB, we seek to honor and celebrate all families and to provide evidence-based content that supports you in your pregnancy and parenting journey. Our goal is to write this article in a way that acknowledges and honors all of our hardships and power. This article makes frequent references to the research on lactation and nursing, and many of the studies we cite use the term breastfeeding. When discussing results from studies, we will use their terms to ensure we are as accurate as possible as we share research with our community. When we are not citing the literature directly, we will use inclusive terminology for lactation and nursing.
Two newer terms that some may not be familiar with yet include chestfeeding and bodyfeeding.
Chestfeeding is an inclusive term for the act of nursing promoted by the NIH (https://bit. ly/3Zbheha), La Leche League USA and Canada (https://bit.ly/3sVtJBb), and by the Academy of Breastfeeding Medicine (Bartick et al. 2021). Chestfeeding can include feeding at the nipple, milk extraction from remaining tissue (in someone who has had top surgery or breast reduction surgery), or the use of supplemental nursing systems (https://bit.ly/3ZtF9bX) (small tubing attached to the breast or chest that allows a baby to feed or simulate feeding at the nipple while also receiving supplemental formula, expressed milk, or donor milk).
Bodyfeeding is another term that encompasses the widest variety of methods parents use to nourish their babies from their bodies, including breastfeeding, chestfeeding, and pumping.
Language changes over time. As our community innovates to find the best ways to inclusively describe ourselves and our bodies, we will keep pace.
See these Evidence Based Birth® Podcasts with experts on this and related topics:
- EBB 116 – Inclusion for Queer and Trans Parent Families with Danie Crofoot (https://ebbirth. com/116)
- EBB 189 – Why Black Lactation Matters and the Importance of Black Breastfeeding Week with IBCLC, Janiya Mitnaul Williams (https://ebbirth.com/189)
- EBB 214 – Supporting Pumping Parents in Lactation with IBCLC, Nichelle Clark (https://ebbirth.com/214)
What is the history of parent-infant separation after birth?
Separation of human parents and newborns is unique to the 20th and 21st centuries and is a complete break from natural human history. In the past, infant survival depended upon close and virtually continuous contact between a baby and its birth parent.
The practice of routinely separating parents and newborns started in the early 1900s, when birth began to move from homes to hospitals. At the time, most birthing people received general anesthesia (medications that induce loss of consciousness) during the pushing phase. This made birthing parents and their babies incapable of interaction after birth. Because mothers could not care for their babies, hospitals created central nurseries to care for newborns, and infants were typically separated from their parents for 24 to 48 hours after birth (Anderson et al. 2004 ).
When did things begin to change?
In 1961, Dr. Berry Brazelton published a classic study showing that general anesthesia during labor was harmful to newborns (Brazelton 1961). As a result, doctors began to move away from using general anesthesia during birth, which resulted in birthing parents and infants being more alert—and capable of interaction—immediately after birth (Anderson et al. 2004).
Most people who give birth by Cesarean today receive regional anesthesia (an epidural, spinal, or combined spinal-epidural) instead of general anesthesia, so these birthing parents, too, are usually alert after giving birth.
Interestingly, when researchers studied human birthing parent-newborn contact in the 1900s and early 2000s, keeping birthing parents and babies together was considered the “experimental” intervention. In contrast, when researchers studied other non-human mammals, keeping mothers and babies together was always the control (or normal) condition, while separating newborns from their mothers was considered “experimental” (Moore et al. 2016).
Kangaroo care
Kangaroo care (https://cle.clinic/3Rp7rSy) (also known as Kangaroo Mother Care or KMC) is the practice of keeping a medically fragile baby skin-to-skin with its birthing parent. Kangaroo care was developed in the late 1970s by Colombian pediatricians and neonatologists Edgar Rey Sanabria and Héctor Martínez Gómez (Abadía-Barrero 2018). At the time, there was an urgent need for low-cost solutions to care for low-birth-weight infants who were born prematurely. Inspired by kangaroos, who keep their young in a pouch for a long period after birth, Drs. Edgar Rey Sanabria and Héctor Martínez Gómez developed Kangaroo care to support low-birth-weight infants without needing incubators or hospitalization (Abadía-Barrero 2018).
The idea was that constant skin-to-skin contact with their parent(s) would help fragile infants regulate their body temperature, until they could learn how to do this on their own (Baley 2015). The doctors reported significant success with Kangaroo care! Data showed Kangaroo care lowered newborn death rates, improved rates of breastfeeding, and prevented infections.
Researchers from outside of Colombia learned about this program and began implementing Kangaroo care in both resource-poor and well-resourced settings. In the late 1990s, the World Health Organization began promoting Kangaroo care as part of its strategy to lower rates of infant death and serious illness (WHO 2003).
Today, Kangaroo care is used around the world, and researchers continue to investigate ways to use the Kangaroo care model for very fragile newborns in NICU settings. The success of Kangaroo care highlights the lifesaving nature of skin-to-skin care!
Skin-to-skin contact and nursing instincts
In the 1970s, Ann-Marie Widstrom, a Swedish nurse-midwife and researcher, observed and charted patterns in the behaviors of babies placed skin-to-skin with their birthing parents immediately after birth (Phillips 2013). Dr. Widstrom discovered that after being placed on the birthing parent’s abdomen, babies (when undisturbed) move through nine distinct phases that include:
- The birth cry
- Relaxation
- Awakening
- Activity
- Resting
- Crawling up to the chest
- Familiarization with the nipple
- Suckling, and then…
- Sleeping
Dr. Widstrom taught that if newborns are provided skin-to-skin contact immediately after birth, they can usually find the nipple, latch, and suckle without assistance. When hospital staff are educated about this normal and instinctive process, they can support the first feeding session without rushing or interfering.
What is routine practice today?
Research overwhelmingly supports skin-to-skin, and hospital practices have been slowly changing.
Depending on the country, rates of skin-to-skin care after a vaginal birth can range from 1% to 98%.
The highest rate of skin-to-skin care is in Croatia (97.8%) and the lowest is in Tanzania (1%) (Abdulghani, Edvardsson, & Amir 2018). Rates of skin-to-skin care also vary by state within the U.S. The percentage of hospitals reporting that they provide ideal immediate postpartum care, including skin-to-skin care, are lowest (78%) in the Southeast states: Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Tennessee, and highest (87%) in the New England states: Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont (CDC 2022).
How does having a Cesarean birth impact skin-to-skin care?
In many hospitals, the routine care after a Cesarean is for the baby to be taken to a warmer in the operating room, where they are examined, cleaned, labeled, weighed, measured, clothed, and swaddled before being shown briefly to the parents. The baby is then taken to a nursery for further assessment and observation in a warmer, while the birthing parent is taken to a separate recovery room, with the separation typically lasting at least one to two hours.
Chances of receiving skin-to-skin care are much lower after a Cesarean than a vaginal birth. For example, in the U.S., the Centers for Disease Control (CDC) tracks skin-to-skin care in hospitals and birth centers, using the Maternity Practices in Infant Nutrition and Care Survey (mPINC™) (https://bit. ly/489BRhO). In 2022, 70% of hospitals said they practice routine, uninterrupted skin-to-skin contact for most babies born vaginally (for at least 1 hour or until the first feeding session). In contrast, only 50% of hospitals said they provide routine skin-to-skin care after a Cesarean.
Cesarean rates can vary from country to country and region to region. Cesarean rates tend to be higher in Latin America and the Caribbean (with an average of 42.8%), West Asia (31.7%), and North America (31.6%) compared to other regions (Betrán et al. 2021). The countries with some of the highest Cesarean rates in the world include Dominican Republic (58.1%), Brazil (55.7%), Cyprus (55.3%), Egypt (51.8%), Turkey (50.8%), and Romania (46.9%) (Betrán et al. 2021). The U.S. Cesarean rate was 32% in 2022, with approximately 1.2 million babies born via Cesarean that year (Hamilton, Martin, & Osterman 2023).
Importantly, the Cesarean rate appears to be increasing globally (Betrán et al. 2021; Boerma et al. 2018). The lower rate of skin-to-skin care with Cesarean means that millions of birthing parents and babies around the world do not receive this best practice.
How often are birthing parents separated from their infants after a Cesarean?
Separation of birthing parents and infants is still common after a Cesarean. In 2013, the last time this data was reported in the U.S., 75% of people who give birth by Cesarean were separated from their babies for at least the first hour (Declercq et al. 2013). In 2007, that figure was even higher, at 86% (Declercq et al. 2007). The standard separation of birthing parents and babies results in a delay in bonding, skin-to-skin contact, and nursing.
Research shows that most of the time when babies are separated from their birthing parents after a Cesarean it is so that the hospital can provide routine care—not because the babies need any kind of special care (Declercq et al. 2007). When an infant is taken to the nursery while their birthing parent recovers separately, it is common for a nurse to give a first feeding of formula (Elliott-Carter & Harper 2012).
Unfortunately, routine separation can harm both birthing parents and infants. In a landmark study published in 2009, researchers randomly assigned birthing parent-baby pairs to several different groups, including one group in which birthing parents and babies were separated for two hours after birth. The researchers found that birthing parents and babies who were separated for two hours had a higher risk of lower parent-infant bonding outcomes one year later, as measured by having a third party (who was unaware of the separation status) review videos of parent-baby interactions (Bystrova et al. 2009).
Today it is highly unlikely that a study like that would ever receive ethical approval. Any future research on parent-baby separation will likely come from animal research. In one animal study, baby horses (foals) were separated from their mothers for one hour after birth (intervention group) or left undisturbed with their mothers (control group). The separation increased the risk for poor bonding and other adverse social outcomes as the foals grew (Henry et al. 2009).
Those of us who have experienced unwanted separation after birth may feel disheartened by these study results. But the good news is that human beings are resilient (including infants!), and although we should avoid being separated from our newborn infants, if possible, this does not mean that we cannot bond with our children after a temporary separation. This research just means we should try to prevent separation whenever possible—and it highlights the importance that hospitals should place on keeping parents and babies together.
The impact of racism on access to skin-to-skin care
Cesarean rates differ for different racial and ethnic communities in the U.S.—meaning that Black and Brown babies are less likely to have skin-to-skin care since they are more likely to experience a Cesarean birth. Here is a breakdown of the Cesarean birth rates in 2022 (Hamilton, Martin, & Osterman 2023):
- Black: 36.8%
- Native Hawaiian or Other Pacific Islander: 32.5%
- Asian: 33.5%
- Hispanic: 31.7%
- White non-Hispanic: 31.1%
- American Indian or Alaska Native 29.5%
Researchers have proposed several theories for why Cesarean rates may differ between communities, often focusing on rates of medical interventions, the relationship between the patient and the healthcare provider, access to prenatal education, and socioeconomic status (Milcent & Zbiri 2018; Sakala et al. 2018; Sakala, Belanoff, & Declerq 2020).
However, these factors alone do not explain the differences in Cesarean rates by race. Experts in racial health disparities such as Dr. Joia Crear-Perry, OB-GYN, and Founder of the National Black Equity Collaborative (which merged with RH Impact) often clarify with the explanation:
“Race isn’t the risk factor – racism is.”
Researchers believe that the medical racism of healthcare providers (both systemic and individual prejudice) has led to higher Cesarean rates among Black and Brown birthing parents—and that this topic demands our attention (Okwandu et al. 2022; Roth & Henley 2012).
To learn more about the impact of racism on pregnancy and childbirth care, visit our Signature Article, Evidence on: Antiracism in Health Care and Birth Work (https://ebbirth.com/antiracism).
Moreover, racism has led to lower rates of exclusive breastfeeding, or the practice of only nourishing a baby with human milk for at least the first six months of life, in Black and Indigenous communities compared to other groups (Mieso et al. 2021). The reasons for this disparity are rooted in histories of enslavement, land theft, racism, racist institutional practices that destabilized family groups, and aggressive marketing of formula or distribution of formula by the government within these communities (Asiodu, Bugg, & Palmquist 2021; Chiang et al. 2021; Davis et al. 2021; Mieso, Burrow, & Lam 2021).
Skin-to-skin care is a free, beneficial practice that could help improve chestfeeding rates. But despite the well-documented relationship between higher Cesarean rates and lower access to skin-to-skin care, there’s very little research that directly addresses access to or the experience of skin-to-skin care among communities of color in the U.S. The one research study we found that investigates this relationship followed the implementation of the Baby Friendly Hospital Initiative (BFHI) (https://www. babyfriendlyusa.org/) and its impact on 39,272 births across 31 hospitals in Mississippi, Louisiana, Texas, and Tennessee (Merewood et al. 2019). In this observational study the researchers wanted to know if implementing the BFHI Ten Steps could lessen racial disparities in nursing that impact Black birthing people and babies.
They found that providing skin-to-skin care after Cesarean was significantly associated with higher rates of starting breastfeeding, and exclusive breastfeeding—with the greatest impact among Black infants (Merewood et al. 2019). Black babies who were roomed in with their parent were more than 1.54 times more likely to exclusively nurse than those who did not, and Black babies who had skin-to-skin care after Cesarean were 1.65 times more likely to nurse exclusively while in the hospital compared to those who did not (Merewood et al. 2019).
So, what can birthing people of color do if they are concerned about access to skin-to-skin care, lowering their risk of Cesarean birth, or gaining enough support in nursing their baby? How can they protect their health and find the support and care they need? A few evidence-based suggestions include:
- Seek out lactation support before giving birth.
- Listen to EBB Podcast 189 about Black Lactation and Black Breastfeeding Week
- Listen to EBB Podcast 214 about pumping with Black IBCLC Nichelle Clark
- Check out Black Breastfeeding Week for resources and events
- Check out Indigenous Milk Medicine Week for resources and events
- Navajo Breastfeeding Coalition
- Native Breastfeeding Coalition of Wisconsin
- Native Breastfeeding Coalition of California
- Seek out care providers and birth workers who are Black, Indigenous, or people of color.
- Listen to EBB Podcast 135 about the importance of Indigenous Birth Workers
- Listen to EBB Podcast 161 featuring Kimberly Sears Allers and her app Irth®
- Listen to EBB Podcast 174 – Evidence on Midwives and check out the resources to find more information about midwifery care and links to Black midwifery care providers.
- You may particularly benefit from Afrocentric group prenatal care, such as the Village Circle Approach™ that is offered at the Ida Mae Patterson Center for Maternal Health and Infant Wellness in Kansas City, Missouri. Listen to EBB Podcast 278 for more details
- Seek out doula support.
- Later in this article we discuss research on the role doulas can play in supporting skin-to-skin after Cesarean.
- Doula care, especially from full-spectrum, community-based doulas who are Black, Indigenous, or people of color, can provide all pregnant families with additional emotional and social support before, during, and after birth.
- See the EBB Signature Article, Evidence on: Doulas to learn more.
- com is a great search directory for Black midwives and doulas.
What are the benefits of skin-to-skin care?
In 2016, Cochrane researchers combined the results from 46 randomized trials that included 3,850 birthing parents and their healthy infants (Moore et al. 2016). Eight of the trials included Cesarean births, and six of the trials included late preterm births (infants born preterm but at greater than 35 weeks’ gestation).
The researchers found strong evidence that skin-to-skin care influences breastfeeding. Birthing parents who had skin-to-skin care with their babies were 24% more likely to still be breastfeeding at one to four months after giving birth, compared to birthing parents who received routine hospital care. They also tended to breastfeed their infants longer, by 64 days on average. When the researchers looked at exclusive breastfeeding (breastfeeding with no use of formula) from six weeks to six months after the birth, they found that the birthing parents who had skin-to-skin care were 50% more likely to exclusively breastfeed.
Babies held skin-to-skin with their birthing parents were 32% more likely to breastfeed successfully during their first feed, and they also had higher blood sugar levels by more than 10 mg/dL. The difference in blood sugar levels is important because infants with low blood sugar may be given formula, a practice that can interfere with bodyfeeding. Overall, the babies that had skin-to-skin care had better combined scores for heart rate, breathing, and oxygen level during the first six hours after birth.
The researchers did not find any differences when they looked at skin-to-skin care beginning within 10 minutes of the birth or after 10 minutes of the birth, or when they compared less than one hour of time spent skin-to-skin to more than one hour. Almost all of the included studies began skin-to-skin care within one hour after the birth. Larger studies are needed to better understand any differences between birth, very early, and early skin-to-skin time, and differences between longer and shorter time spent skin-to-skin.
In a 2018 review, researchers suggest that while early skin-to-skin care is rarely provided to premature or ill newborns, that it may in fact benefit them (Almgren 2018). Researchers have found higher cortisol (stress) levels in infants not held by their birthing parents after birth (Elverson et al. 2012). And a large study in Canada found that critically ill babies had a higher mortality rate when they were separated from their birthing parent after birth (Ray et al. 2012).
In contrast, skin-to-skin care can help a sick or premature newborn stabilize through reducing stress, using the parent’s body to provide consistent warmth, comfort, and nourishment (Almgren 2018; Elverson et al. 2012).
Research has also shown that skin-to-skin care can greatly improve the birth experience. The care that birthing people receive can have long lasting implications for their relationships and their psychological health across the life course, so it is important to pay attention to the experience of childbirth and to support practices that improve that experience (Deys, Wilson, & Meedya 2021).
In a 2019 study of more than 3,000 participants, researchers found that people who had a Cesarean and held their child shortly after birth reported a better birth experience overall than those who birthed vaginally (Brubaker et al. 2019). This team of researchers also found that birthing people whose care team included a doula or midwife were more likely to see and hold their newborn immediately after birth (Brubaker et al. 2019). And in a study with more than 1,371 Israeli women, skin-to-skin care had the greatest positive impact on satisfaction among those who had a Cesarean (Kahalon, Preis, & Benyamini 2021).
To summarize, the benefits of early skin-to-skin care include:
For birthing parents:
- Longer duration of breastfeeding.
- More likely to exclusively breastfeed.
- Less chest engorgement/pain at three days.
- Less anxiety three days after birth.
- Higher satisfaction—birthing parents who held their baby skin-to-skin were six times more likely to want the same care vs. those who held their baby swaddled.
For babies:
- More effective suckling during the initial breastfeeding session.
- Less crying– babies who received skin-to-skin care were 12 times less likely to cry during the observation period.
- Heart rate, breathing, and oxygen levels were more likely to remain stable.
- A beneficial increase in blood sugar.
The benefits of skin-to-skin care are so clear that the World Health Organization recommends that ALL newborns receive skin-to-skin care, including low-birthweight and premature babies (WHO 2022). Skinto-skin should begin immediately after birth and continue uninterrupted for at least one hour or until the first feeding session for birthing parents who are breastfeeding or chestfeeding.
Are there any potential harms to keeping birthing parents and babies together for skinto-skin care?
The only risk to early skin-to-skin care is a rare event called sudden unexpected postnatal collapse (SUPC). This is when a seemingly healthy infant becomes rapidly unstable within the first two hours after the birth, often during the first feeding session. This event happens in three to five infants out of 100,000 births. Zero to 1.1 deaths due to SUPC are thought to occur for every 100,000 births (Moore et al. 2016).
SUPC is most likely to occur when an infant has an internal health problem, like an infection or heart defect, combined with another exposure, such as pain medication or magnesium sulfate medication during labor, or risky positioning after the birth (Ferrarello & Carmichael 2016). Studies have found that 74% of cases occurred while the baby was lying face down during skin-to-skin contact with their birthing parent, and in 77% of cases, the birthing parent or both parents were alone with the newborn at the time of the episode (Ferrarello & Carmichael 2016; Herlenius & Kuhn 2013).
Researchers have proposed a few safety measures to decrease the risk of SUPC during skin-to-skin care (Ferrarello & Carmichael 2016):
- Increase the time that a nurse or midwife observes the birthing parent-infant pair during the first two hours after birth.
- Educate the parents and the doula (if present) to recognize abnormal newborn appearance and behaviors—such as pale or bluish skin color, difficulty breathing, or limp muscle tone—and delay the use of smartphones until the first two hours after birth.
- Elevate the head of the birthing parent’s bed to between 35 degrees and 80 degrees so that the baby isn’t lying flat down on the birthing parent’s chest.
- Educate the birthing parent about safe breastfeeding and check frequently to be sure that the baby’s neck is straight, and that nose and mouth are not blocked.
Hospitals can develop their own safety protocols and take advantage of existing assessment tools that can help them to identify and respond quickly to infants that become unstable while skin-to-skin (Davanzo et al. 2015; Ludington-Hoe & Morgan 2014).
What about after a Cesarean—are there any risks to keeping birthing parents and babies together after a Cesarean?
Some parents may not be able to independently care for their infants immediately or for several hours after a Cesarean. For example, if you received strong sedatives or were sleep-deprived for many hours before the Cesarean, you may need supervision or assistance in caring for your newborn.
Your level of awareness and ability to remain awake when caring for and feeding an infant must be assessed and closely monitored by nursing staff, especially when a Cesarean follows a prolonged labor or when sedative medicines were given (Mahlmeister 2005).
Can Cesareans be performed in a way that encourages skin-to-skin care?
In a popular 2015 YouTube video, Sarah Cooke was recorded giving birth to her son via Cesarean. The drape was lowered so Sarah could watch as the doctor lifted her son’s head out of the incision in her uterus. Then the baby seemed to join Sarah in the birthing process, helping ‘birth himself’ by wiggling onto her body. This video, viewed over 2 million times, received attention from publications like The Telegraph, as an alternative approach to Cesareans.
What made this birth so special that so many people tuned in to watch? Well, millions of people around the world have given birth by Cesarean, and some of them have told us that they wish they could have had a gentler birth experience, just like Sarah’s.
Smith, Plaat, & Fisk describe a Natural Cesarean as one in which the parents are involved as active participants in the birth and the baby is transferred directly onto the birthing parent’s chest for early skin-to-skin (2008). This type of Cesarean is sometimes called a gentle Cesarean or a family-centered Cesarean (Magee et al. 2014; Schorn et al. 2015). The idea is to mimic a vaginal birth as much as possible, with pauses that allow the birthing parent and family to see the baby’s head emerge first. Then the rest of the baby’s body slowly emerges through the surgical incision, until the baby is resting on the birthing parent’s body (instead of being whisked away to a warmer) (Smith, Plaat, & Fisk 2008).
When preparing for a gentle Cesarean, health workers make space on the birthing parent’s body to receive the infant by carefully arranging monitors and leads. They also prepare warm towels to help the baby stay warm and assign a specific health care worker a role in assisting with immediate skin-to-skin in the operating room. Delayed cord clamping can also be practiced during this type of Cesarean (Smith, Plaat, & Fisk 2008). Techniques may vary depending on the hospital, but the main focus is to put the infant on the birthing parent’s skin as soon as possible after birth, and to avoid unnecessary separation of the infant and parent(s) (Magee et al. 2014).
We do not have much research on gentle Cesareans, but there is plenty of research on one important part of this practice—and that is skin-to-skin in the operating room!
What is the evidence for skin-to-skin care specifically for babies who are born by Cesarean?
Meta-analysis of randomized, controlled trials
Researchers have combined all the results from randomized trials on this topic into one large study, called a meta-analysis. The most important meta-analysis on this subject was published by Moore et al. in 2016, with a total of 46 studies.
Out of all the studies, 8 trials included participants who gave birth by Cesarean. The birthing parents received epidurals or spinals in seven of the trials and general anesthesia (“put to sleep”) in one trial. None of the trials included emergency Cesareans, and all the infants were full term. Most of the time, skin-to-skin care was started in recovery room at about 50 minutes after the birth. Only one study started the skin-to-skin care in the operating room. Skin-to-skin care was usually provided for 30 to 80 minutes.
The researchers found that skin-to-skin care resulted in several benefits after a Cesarean birth. The infants who received skin-to-skin care were 22% more likely to still be breastfeeding one and four months after the birth. Seven out of eight studies also found an increase in exclusive breastfeeding at hospital discharge. Some parents also reported less pain after their Cesarean, but the evidence was not strong enough to show a clear effect on pain.
Reviews of observational research
In a more recent review of observational research, researchers looked at 13 studies that focused on maternal and infant outcomes of skin-to-skin after Cesarean birth (Frederick, Fry, & Clowtis 2020). They included six prospective studies, four retrospective chart reviews, and three qualitative studies. The researchers found a decrease in the biomarkers associated with stress, as well as an increase in hormones associated with buffering stress (Frederick, Fry, & Clowtis 2020). Biomarkers are characteristics of your body, like blood pressure or height, that can be measured. When it comes to stress, biomarkers can include the level of cortisol, the stress hormone, in your blood. This suggests that having skin-to-skin immediately after a Cesarean may protect both birthing parents and infants from the hormones associated with stress.
The researchers found no significant differences in temperature, Apgar scores, oxygen levels, or heart rate in infants who had immediate skin-to-skin after Cesarean birth (Frederick, Fry, & Clowtis 2020). The Apgar score (sometimes called the newborn Apgar score) is an assessment tool that healthcare providers use to check the baby’s health shortly after birth (https://cle.clinic/3Lfhl5l). The Apgar score is used to determine whether or not a baby might need to be resuscitated or is having other health issues that might require closer monitoring or intervention.
The benefits to birthing parents who have skin-to-skin care after a Cesarean birth go beyond improved breastfeeding and reducing pain. In another review of 13 studies from around the world, researchers found that skin-to-skin care after Cesarean has a positive impact across cultures and across healthcare settings (Deys, Wilson, & Meedya 2021).
For example, in one study of birthing parents who had skin-to-skin care after Cesarean, participants reported that the skin-to-skin care improved their birth experience and helped them feel secure and that their baby was safe (Bertrand and Adams 2020). For those who had an unscheduled Cesarean, they credited skin-to-skin care with helping them cope with the unexpected way they gave birth (Bertrand and Adams 2020). It is important to note that the people in this study were not necessarily supported in seeking skin-to-skin, with participants noting that they had to advocate for themselves, sometimes even demanding skin-to-skin care. For those who had skin-to-skin care offered to them by their health care team, they reported feeling supported.
Individual studies on skin-to-skin care for babies born by Cesarean
Some individual studies have highlighted other benefits of immediate skin-to-skin care after a Cesarean, and we review their findings below:
Small, randomized trial found that skin-to-skin care led to earlier breastfeeding
In 2012, Velandia et al. randomly assigned 37 families planning a Cesarean to immediate skin-to-skin care with the birthing parent (who all self-identified as mothers) or immediate skin-to-skin care with the non-birthing parent (who all self-identified as fathers). In both groups, the baby was placed skin-toskin on the mother’s chest within one minute after birth and stayed there for five minutes. Afterwards, the baby either remained there for 25 more minutes or was switched to the father’s chest for 25 minutes. After this time, all the babies did skin-to-skin with their mothers for an additional 90 minutes.
Babies who spent skin-to-skin time with mothers breastfed significantly earlier than babies who had skin-to-skin with their fathers. There were no adverse effects reported. This study was limited by its lack of a true control group and because they did not report any measurements on infant temperature, breathing, or heart rate.
Larger, randomized controlled trial found that immediate skin-to-skin made a difference in breastfeeding outcomes
The largest randomized, controlled trial to examine immediate skin-to-skin care included 366 people having an elective Cesarean for a single baby at 37 to 42 weeks of pregnancy (Gregson et al. 2016). The outcome that the researchers were most interested in was breastfeeding rates, so families who expressed a desire to formula feed their infants were excluded from the study.
Participants were randomly assigned to immediate skin-to-skin care in the operating room (182 families) or standard care (187 families). The group assigned to immediate skin-to-skin care received a KangaWrap Kardi to wear under the operation gown. The KangaWrap Kardi was a simple garment that was designed to help facilitate skin-to-skin care after Cesarean (this product no longer seems to be available). After birth, each baby was placed immediately on the birthing parent’s chest, and families were encouraged to keep the baby skin-to-skin as much as possible during the first 48 hours. For ethical reasons, the standard care group also received the baby after birth and birthing parents were encouraged to have at least one hour of skin-to-skin time.
Not surprisingly, most participants assigned to the standard group also wanted to spend a lot of time skin-to-skin with their newborns. Because of this crossover, or ‘contamination’ of the standard care group, both groups spent a similar amount of time doing skin-to-skin.
When data from both groups were combined, they found that the length of time spent skin-to-skin was directly linked to the rate of continuing to breastfeed at 48 hours—with longer time spent skin-toskin leading to a higher rate of continuing to breastfeed at 48 hours. However, we don’t know if more time spent skin-to-skin was a direct cause of breastfeeding success, or if the mothers who were more motivated to breastfeed chose to spend more time skin-to-skin.
This study provides evidence that most birthing parents desire skin-to-skin time with their newborns as soon as possible after Cesarean, that it is possible to safely practice skin-to-skin care in the operating room, and that more time spent skin-to-skin may benefit breastfeeding.
Small, randomized trial found that a gentle Cesarean approach and immediate skin-to-skin improved breastfeeding outcomes.
In 2016, Armbrust et al. randomly assigned 205 people at more than 37 weeks’ gestation who were planning a Cesarean to either immediate skin-to-skin (along with a gentle Cesarean approach) or routine separation.
In the skin-to-skin group, a gentle Cesarean approach was used, which the researchers chose to call a Charité Cesarean. The surgical drape was lowered so that the family could see the birth, the infant was slowly delivered (also called “walked” out of the uterus) by the doctor, and the non-birthing partner was given the option to cut the umbilical cord. The naked infant was briefly examined and placed on the mother’s bare breast and covered by a warm blanket. The baby remained skin-to-skin with the birthing parent for the rest of the surgical procedure and into recovery—a total of one hour or more.
In the routine separation group, the baby was taken away immediately for an assessment. The article does not specify when the babies in this group were returned to the parents.
The study found that parents who experienced the gentle Cesarean and immediate skin-to-skin care rated their birth experience much better than the group that had a routine Cesarean followed by immediate separation. Rates of breastfeeding were higher in the group that received immediate skin-toskin (81 vs. 69%), and they reported fewer problems breastfeeding. There were no adverse outcomes or differences in Apgar scores between groups.
Small, randomized trial found that immediate skin-to-skin after Cesarean may reduce stress hormones in birthing parents
A 2019 study randomly assigned 40 families into two groups: one group began skin-to-skin care immediately after Cesarean in the operating room, and one group received standard post-Cesarean care, where they could not begin skin-to-skin until the umbilical cord had been cut, surgery had been completed, and they had transferred to the recovery room bed, but could begin while still in the operating room (Crenshaw et al. 2019).
The researchers measured each birthing parent’s heart and breathing rate, oxygen saturation, temperature, blood pressure, and the amount of cortisol (the stress hormone) in their saliva to learn more about the effects of each approach to Cesarean (Crenshaw et al. 2019). They took these measurements before surgery, about 20 minutes after birth, one hour after birth, and two hours after birth (Crenshaw et al. 2019).
Results showed that birthing parents in the skin-to-skin care group had lower levels of stress hormones and higher blood oxygen levels compared to those who were separated from their infants. They found no major differences in newborn temperatures between groups. Although newborns in the skin-to-skin groups had initially lower temperatures in the operating room, their temperatures remained within the normal range (Crenshaw et al. 2019).
Small, randomized trial found that very preterm babies benefited from skin-to-skin very early after
Cesarean birth
A study in Norway looked at the impact of skin-to-skin on very preterm infants born vaginally and via Cesarean to learn if this could benefit these fragile newborns (Kristoffersen et al. 2023). The study included 108 infants born between 28 to 31 weeks’ gestation, 62 of whom were born via Cesarean.
All the babies were first placed in a warming resuscitation unit for assessment and stabilization before being randomized into one of two groups:
- Infants in the standard care group (57 babies) were immediately transferred to an incubator to be assessed before being moved to the NICU.
- Infants in the skin-to-skin group (51 babies) were initially placed in the incubator for stabilization and assessment, and then as quickly as possible placed on the birthing parent’s chest. These infants were able to remain skin-to-skin for up to two hours before being transferred to the NICU in an incubator.
The researchers found that rates of hypothermia (low body temperature) and hyperthermia (high body temperature) were lower in the skin-to-skin group than in the group placed in an incubator after birth (4% vs 7%; 26% vs. 47%) (Kristoffersen et al. 2023). The infants who received skin-to-skin care were also more likely to be discharged early to home care. Over 50% of the infants in this study were born via Cesarean, leading researchers to suggest that it is safe for very fragile infants to receive very early skinto-skin care, whether they are born vaginally or via Cesarean.
Observational study suggests that skin-to-skin during Cesareans might decrease the likelihood of transfer to NICU
In a medical records study, researchers looked at four years of non-emergency Cesareans for infants born at 37 to 42-weeks’ gestation at a single hospital in the U.S. (Schneider et al. 2017). The first two years of data were from before the hospital began using immediate skin-to-skin during Cesarean, and the last three years of data were from after a new skin-to-skin care practice went into effect.
The researchers found that fewer newborns were transferred to the NICU for observation after the skinto-skin practice began (1.8 vs. 5.6%). There were no other policy changes over this time that could have impacted the number of babies sent to the NICU. The authors point out that fewer babies being sent to the NICU for observation could reduce costs for hospitals, since NICU observations are not always reimbursable.
Quality improvement studies of skin-to-skin after Cesarean
There are quite a few quality improvement reports in the literature in which hospitals describe implementing immediate skin-to-skin care during a Cesarean (Brady, Bulpitt, & Chiarelli 2014; Boyd 2017; Hung & Berg 2011; Lanning et al. 2019; Moran-Peters et al. 2014; Smith, Plaat, & Fisk 2008; Sundin 2015). Quality improvement (QI) in healthcare refers to the process of using data to begin new processes or systems for providing care—and these new processes or systems are intended to improve patient outcomes, improve staffing, or address clinical problems.
In these QI reports on immediate skin-to-skin care after Cesarean, hospitals reported seeing improvements in breastfeeding rates as well as lower pain perception and anxiety, and higher satisfaction for birthing people. They found no adverse effects from using immediate skin-to-skin care in the operating room.
In 2012, researchers at a Texas hospital carried out an “intervention” to help staff increase the rates of immediate skin-to-skin care. After formal training sessions on the benefits of skin-to-skin, the researchers videotaped 11 births (five vaginal, six Cesarean) in which immediate skin-to-skin was used, and then they showed these videos to staff. The videos helped the staff discuss how they could make the process work smoother. Before the intervention, about 58% of birthing parents and babies had immediate skin-to-skin care. In the months afterwards, the rate of immediate skin-to-skin care increased to 83%. Almost all the increase was due to birthing parents who gave birth by Cesarean having immediate skin-to-skin in the operating room (the hospital did not routinely do skin-to-skin in the operating room before) (Crenshaw et al. 2012).
In a 2019 QI project, volunteer doulas at a labor and delivery unit in the U.S. were trained on how to help provide skin-to-skin care after Cesarean (Lanning et al. 2019). Researchers found that among 58 infant/ parent couples who had a scheduled Cesarean, all were able to initiate skin-to-skin care, with about 11 minutes (give or take 9 minutes) passing between birth and the start of skin-to-skin care. One-third of the infant/parent couples were transferred to recovery rooms while maintaining skin-to-skin care. The presence of the doulas made it easier to provide skin-to-skin care and had a positive impact on the birth experience of participants (Lanning et al. 2019).
I would like to have skin-to-skin care as soon as possible after my Cesarean, but my hospital says they won’t let me. Why is that?
There are a few reasons that hospitals resist skin-to-skin care after Cesarean birth. Many hospital staff perceive that skin-to-skin care may be “risky” to the birthing parent or infant. They may worry that skin-to-skin care in the operating room may pose the risk of hypothermia (low body temperatures) for a newborn baby. Some staff may also think that the logistics are just too difficult to provide this type of care. And finally, skin-to-skin care in the operating room may be in conflict with the culture of the medical institution.
Here are some of the potential perceived barriers to skin-to-skin care after a Cesarean (Balatero, Spilker, & McNiesh 2019; Hung & Berg 2011; Smith, Plaat, & Fisk 2008):
- Concern that the birthing parent cannot hold the baby after Cesarean safely:
- The birthing parent may not be capable of holding the baby due to nausea or other symptoms— in this case, another family member would need to do skin-to-skin with the baby.
- Concern that the infant may to be too slippery to hold or lay safely on the operating table with their birthing parent.
- Concern that skin-to-skin care after Cesarean requires too many staff:
- Some hospitals may require a designated baby nurse to be in the operating room or the recovery room (in addition to the birthing parent’s nurse) so a shortage of nurses may prohibit early skinto-skin care.
- Nurses may face a new requirement to learn to ‘scrub-in’ for Cesareans to safely receive the baby through the drape.
- Belief that skin-to-skin care interferes with ‘business as usual’ in the operating room:
- The birthing parent’s heart monitor stickers need to be placed on their sides, to leave a spot open on their chest for the baby.
- The birthing parent’s gown needs to be placed so that it easily opens for the baby to lay on their bare chest.
- The birthing parent’s blood pressure cuff and IV needs to be placed on the non-dominant arm.
- The birthing parent’s oxygen monitor needs to be put on their toe instead of their finger.
- The baby needs to be dried and covered with multiple warm blankets (potentially bubble wrap) and a cap.
- If the skin-to-skin time is done very early (in the OR), the baby may need to be laid crosswise across the birthing parent’s upper chest, above the sterile drape.
- Routine procedures, such as weight, measurement, and baby eye drops, need to be delayed.
- Other routine baby procedures (Apgar scores, assessment, placing the ID bracelet) need to be done on the birthing parent’s chest.
- Bathing needs to be delayed, with priority given to the skin-to-skin time.
Now that we know the perceptions, it is time to consider what the research actually says. We outline some of the research on these perceived barriers below.
Baby’s temperature
One of the main perceived barriers to providing skin-to-skin care after a Cesarean is because hypothermia (low temperature) in babies is more common after a Cesarean. In fact, many healthcare providers cite this as a safety concern (Balatero, Spilker, &McNiesh 2019).
Babies who are born via Cesarean are at higher risk of hypothermia because the operating room temperature is kept quite cold, birthing parents may have a lower body temperature during a Cesarean, and babies were exposed in utero to medications that may affect their temperature (Moore et al. 2016).
However, research evidence suggests that babies who undergo skin-to-skin care for 30 to 50 minutes after a Cesarean are NOT at higher risk for hypothermia compared to infants who are kept in a warmer (Gouchon et al. 2010; Nolan & Lawrence 2009).
If a baby is not able to maintain its temperature during skin-to-skin with the birthing parent, babies can still be held skin-to-skin with the non-birthing partner or another family member after a Cesarean (Erlandsson et al. 2007). In a 2018 feasibility study that enrolled 91 infant-parent dyads, researchers at a hospital in northern California found that 53% (54) of infants born via elective Cesarean who received skin-to-skin care either maintained their body temperature or even saw an increase in body temperature (Bilner-Garcia, Spilker, & Goyal 2018). While 40% (44) of the infants in this study had a decrease in temperature, only 4 had a decrease in temperature significant enough to require an intervention that interrupted skin-to-skin care (Bilner-Garcia, Spilker, & Goyal 2018).
Time and space
A lack of space in the operating room is often listed as a barrier to skin-to-skin care in the operating room (Balatero, Spilker, & McNiesh 2019). Length of time spent in the operating room is another logistical concern for immediate skin-to-skin care. One study of 110 people who had a planned Cesarean found that skin-to-skin care in the operating room did not impact time spent in the room (Cuerva et al. 2022). The study did see an increase in the rate of breastfeeding at hospital discharge among those who had immediate skin-to-skin vs. those who did not have immediate skin-to-skin (74% vs. 57.4%) (Cuerva et al. 2022).
Maintaining the sterile field
Another perceived barrier is that it seems like it might be more difficult to maintain a sterile field or prevent incision infections during skin-to-skin time (Balatero, Spilker, & McNiesh 2019; Baley 2015). In one multi-center study that included 243 people who had an elective Cesarean, researchers found no difference in surgical site infections between those who underwent a gentle Cesarean, and those who did not (Brongeest et al. 2019).
In another study of 650 birthing people who had elective and emergency Cesareans, researchers compared those who had immediate skin-to-skin care (285) with those who received standard care after Cesarean (365) (Posthuma et al. 2017). They found that rates of infection were low in both groups, with 2.1% (6 participants) reporting surgical site infections in the skin-to-skin group compared to 1.6% (6 participants) in the standard care group (Posthuma et al. 2017). The skin-to-skin group did end up with two cases of sepsis (blood infection), but both were unrelated to the skin-to-skin care (retained placenta and gallbladder infection).
There were no differences in blood loss and no differences in the need for blood transfusion. The length of time spent in surgery and the average recovery time were both shorter in the immediate skin-toskin group. Of the infants in the study, those who received immediate skin-to-skin care had fewer admissions to the NICU (9.5% vs. 18%), and fewer suspected infections (2.0% vs 7.3%). The rate of low Apgar scores at 5 minutes after birth were not significantly different between groups (1.5 to 2.4%). Overall, these results suggest that immediate skin-to-skin care does not increase the risk of infection or lengthen the time spent in surgery (Posthuma et al. 2017).
Hospital culture
Probably the biggest barrier to skin-to-skin care after a Cesarean is the culture of the operating room itself. Several clinicians have discussed how they began using immediate skin-to-skin care (within 30 minutes after birth) in their hospitals’ operating rooms (Hung & Berg 2011; Smith, Plaat, & Fisk 2008). The authors noted that, at first, hospital staff were skeptical, reluctant, and afraid to change their routine habits and behaviors. But after seeing the benefits of this family-friendly procedure, staff became supportive of the change.
For change to take place in a hospital, it requires a shift from “how it has always been done” to what the current evidence shows is best for families. This change can be helped along by dedicated nurses or physicians who are seen as leaders by their peers.
In Michigan, Dr. Tami Michele successfully led the charge to convert Spectrum Health Gerber Memorial hospital over to routine skin-to-skin care after Cesarean. Dr. Michele started by approaching the anesthesia providers, since their workspace at the head of the birthing parent’s bed was most affected by the changes in patient monitoring. She provided information on the benefits of skin- to-skin care after Cesarean and details about how procedures would change. Dr. Michele presented the change from the perspective of improving the Cesarean patient’s experience. She brought everyone to the table— past patients, doulas, nurses, anesthesia providers, lactation consultants, clinical supervisors, childbirth educators, marketing directors, surgical staff, and hospital administration—so that the entire team felt ownership of the changes they were about to create.
It’s important to address everyone’s concerns to get staff completely on board with the new way of providing care. For example, physicians may think that they need the newborn’s weight right away to complete the patient’s chart. However, the record could be completed later or documented as “weight pending due to skin-to-skin.” Education for staff can be helpful to decrease anxiety around making changes (Personal correspondence, Michele 2017).
Is it possible for hospitals to keep birthing parents and babies together in recovery after a Cesarean?
Yes. For example, at Spectrum Health Gerber Memorial hospital in Michigan, birthing parents are admitted to the room they will be in during their hospital stay for a planned cesarean. The preoperative procedures are done there. After the surgery, the parents and baby return to that same room for immediate post-operative recovery. Other family and friends are asked to wait to visit until the surgical recovery time is completed. The birthing parent and partner continue skin-to-skin and initiate breastfeeding (if the baby had not already started breastfeeding during the surgery). The baby only goes to the nursery if there is a medical emergency (Personal correspondence, Michele 2017).
Another interesting quality improvement report was published by Elliott-Carter & Harper in 2012. This report described how nurses at Woman’s Hospital in Baton Rouge, Louisiana led a switch from routine separation after Cesareans to keeping birthing parents and babies together. The hospital was motivated to change for several reasons, including a desire to stay competitive with other hospitals and repeated requests from clients to not be separated from their babies. Perhaps most compelling, the staff felt it was simply “not fair” that birthing parents who gave birth vaginally were allowed to stay with their babies, while birthing parents who had Cesareans were automatically separated from their babies. The Cesarean rate at Woman’s hospital was 40%, and they have more than 8,000 births per year. So, making this change affected 3,200 families per year.
One of the first things the hospital did was put together a leadership team to plan for the change. A major challenge for this team was finding a space that was large enough for birthing parents and babies to recover together after a Cesarean. They ended up choosing overflow labor and delivery suites that were big enough for this purpose. They also modified the existing recovery room (Post Anesthesia Care Unit, or PACU) so that it could be used in case the overflow rooms were full.
The team had to train the recovery (PACU) nurses in neonatal resuscitation. They placed baby blankets in the heated blanket warmer and stocked appropriate medications for both birthing parents and babies in each room.
Perhaps most importantly, staff made a commitment to provide care where the birthing parents and babies were. Although taking the baby to the nursery was easier and more convenient for the staff, they realized that keeping parents and babies together was best for everyone.
In the first year after starting this project, the percentage of infants who were separated from their birthing parents dropped from 42% to only 4%. Nurses stated that everyone was extremely satisfied with the change—including staff, physicians, and families. Nurses also reported that birthing parents can have skin-to- skin contact earlier, and that the first breastfeeding session goes smoother.
As nurses from the Woman’s Hospital said, “If a hospital that delivers 8,000 infants annually can find a way to decrease the separation of birthing parents and newborns, concerned nurses everywhere should be able to implement this type of care.”
In summary, the research we have so far demonstrates that both immediate and very early skin-to-skin care after a Cesarean is safe and beneficial—including skin-to-skin care that is started in the operating room. For parents interested in any form of bodyfeeding, from nursing to pumping, skin-to-skin care after Cesarean can help support that plan.
The low rates of skin-to-skin care after Cesarean and reports from researchers suggest that families and hospital staff face multiple barriers to skin-to-skin care after Cesareans. However, evidence has shown that it is possible—and best practice—for birthing parents and babies to stay together after a Cesarean. Hospitals not currently supportive of skin-to-skin care after Cesarean should act immediately to make the changes necessary to support this best practice.
If a hospital staff member tells you that it is “impossible” for you to recover together with your baby after a Cesarean, that statement is false. Making the switch from routine separation to keeping parents and babies together is possible—many hospitals have already done so. Although separating parents and babies after a Cesarean may have been perceived as more “convenient” for staff in the past, in the end, keeping birthing parents and babies together after a Cesarean has been shown to safe, evidence-based, and beneficial.
Here at EBB, we teach our Childbirth Class students that it may be helpful to ask your provider these questions during a prenatal visit:
“What is your Cesarean rate?”
“If I have a Cesarean, is it possible to have skin-to-skin care with my baby in the operating room?”
“Are parents and babies able to do their post-op recovery in the same room?”
If skin-to-skin care is a high priority for you and your chosen facility does not support skin-to-skin care
after a Cesarean (or if they separate birthing parents from their babies during recovery), you may want
to consider looking at other birth options in your community, if possible. You can also print off a copy of the handout of this article and share it with your providers.
Ultimately, as more families, birth workers, and health care workers request skin-to-skin care in the operating room, more facilities will begin to offer family-centered Cesarean care
References:
- Abadía-Barrero, C. E. (2018). “Kangaroo Mother Care in Colombia: A Subaltern Health Innovation against For-profit Biomedicine.” Med Anthropol Q 32(3): 384–403. https://pubmed.ncbi.nlm.nih.gov/29363780/
- Abdulghani, N., Edvardsson, K., & Amir, L. H. (2018). “Worldwide prevalence of mother-infant skin- to-skin contact after vaginal birth: A systematic review.” pLoS One 13(10): e0205696. https://doi.org/10.1371/journal.pone.0205696
- Almgren, M. (2018). “Benefits of skin-to-skin contact during the neonatal period: Governed by epigenetic mechanisms?” Genes Dis 5(1): 24-26.
- American College of Nurse Midwives (ACNM). (2023). “Position Statement: Primary Cesarean Birth by Request.” . Accessed August 16, 2023.
- American College of Obstetricians and Gynecologists Committee on Obstetric Practice, Breastfeeding Expert Work Group [ACOG]. (2018). “ACOG Committee Opinion Number 756, Optimizing Support of Breastfeeding as Part of Obstetric Practice.” Obstet Gynecol 132(4): e187–e196.
- Armbrust, R., Hinkson, L., von Weizsacker, K., et al. (2016). “The Charite cesarean birth: a family orientated approach of cesarean section.” Journal of Maternal-Fetal & Neonatal Medicine 29(1):163–168. [3180063].
- Anderson, G. C., Radjenovic D., Chiu, S. H., et al. (2004). “Development of an observational instrument to measure mother-infant separation post birth.” J Nurs Meas 12(3): 215-234.
- Bartick, M., Stehel, E.K., Calhoun, S.L., Feldman-Winter, L., Zimmerman, D., Noble, L., Rosen-Carole, C., Kair, L.R., and The Academy of Breastfeeding Medicine. (2021). “Academy of Breastfeeding Medicine Position Statement and Guideline: Infant Feeding and Lactation-Related Language and Gender.” Breastfeed Med 16(8): 1–4.
- Asiodu, I. V., Bugg, K., & Palmquist, A. E. L. (2021). “Achieving Breastfeeding Equity and Justice in Black Communities: Past, Present, and Future.” Breastfeed Med 16(6): 447–451. https://pubmed.ncbi.nlm.nih.gov/33979550/
- Balatero, J. S., Spilker, A. F., & McNiesh, S. G. (2019). “Barriers to Skin-to-Skin Contact after Cesarean Birth.” MCN Am J Matern Child Nurs 44(3): 137-143.
- Baley, J., Committee on Fetus and Newborn. (2015). “Skin-to-Skin Care for Term and Preterm Infants in the Neonatal ICU.” Pediatrics 136(3): 596–599.
- Bertrand, K. M. & Adams, E. D. (2020). “A Study of Skin-to-Skin Care During Cesarean Birth: A Mother’s Experience.” J Perinat Educ 29(1): 50–58. 10.1891/1058-1243.29.1.50
- Betrán, A. P., Ye, J., Moller, A., et al. (2016). “Trends and projections of caesarean section rates: global and regional estimates.” BMJ Glob Health 6(6): e005671.
- Bilner-Garcia, R., Spilker, A., & Goyal, D. (2018). “Skin to Skin Contact: Newborn Temperature Stability in the Operating Room.” MCN Am J Matern Child Nurs 43(3): 158–163. 10.1097/NMC.0000000000000430
- Boerma, T., Ronsmans, C., Melesse, D. Y., et al. (2018). “Global epidemiology of use of and disparities in caesarean sections.” Lancet 392(10155): 1341–1348.
- Bollag, L., Lim, G., Sultan, P., et al. (2021). “Society for Obstetric Anesthesia and Perinatology: Consensus Statement and Recommendations for Enhanced Recovery After Cesarean.” Anesth Analg 132(5): 1362–1377. 10.1213/ANE.0000000000005257
- Boyd, M. M. (2017). “Implementing Skin-to-Skin Contact for Cesarean Birth.” AORN J 105(6): 579–592.
- Brady, K., Bulpitt, D., & Chiarelli, C. (2014). “An interprofessional quality improvement project to implement maternal/infant skin-to-skin contact during cesarean delivery.” J Obstet Gynecol Neonatal Nurs 43(4): 488–496.
- Brazelton, T. B. (1961). “Effects of maternal medication on the neonate and his behavior.” Journal of Pediatrics 58: 513–518.
- Brongeest, K., Wolters, V. E. R. A., Freeman, L. M., et al. (2019). “Short report: Post-operative wound infections after the gentle caesarean section.” Eur J Obstet Gynecol Reprod Biol 241: 131–132.
- Brubaker, L. H., Paul, I. M., Repke, J. T., et al. (2019). “Early maternal-newborn contact and positive birth experience.” Birth 46(1): 42–50.
- Bystrova, K., Ivanova, V., Edhborg, M., et al. (2009). “Early contact versus separation: effects on mother-infant interaction one year later.” Birth 36(2): 97–109.
- Centers for Disease Control and Prevention (2022). “Maternity Practices in Infant Nutrition and Care (mPINC™) Survey.” Accessed online August 3, 2023. 11, 2017.
- Chiang, K. V., Li, R., Anstey, E., et al. (2021). “Racial and Ethnic Disparities in Breastfeeding Initiation — United States, 2019.” MMWR Morb Mortal Wkly Rep 70(21): 769–774.
- Crenshaw, J. T., Cadwell, K, Brimdyr, K., et al. (2012). “Use of a video-ethnographic intervention (PRECESS Immersion Method) to improve skin-to-skin care and breastfeeding rates.” Breastfeed Med 7(2): 69–78.
- Crenshaw, J. T., Adams, E. D., Gilder, R. E., et al. (2019). “Effects of Skin-to-Skin Care During Cesareans: A Quasiexperimental Feasibility/Pilot Study.” Breastfeed Med 14(1): 731–743.
- Cuerva, M. J., Carbonell, M., Boria, F., et al. (2022). “Influence on operative time of immediate skin-to-skin care in low-risk primary cesarean births for breech presentation: Retrospective cohort study.” Birth Epub ahead of print: 1–7.
- Davanzo, R., De, C. A., Paviotti, G., et al. (2015). “Making the first days of life safer: preventing sudden unexpected postnatal collapse while promoting breastfeeding.” Journal of Human Lactation 31(1):47–52.
- Davis, C., Villalobos, A. V. K., Turner, M. M., et al. (2021). “Racism and Resistance: A Qualitative Study of Bias As a Barrier to Breastfeeding.” Breastfeed Med 16(6): 417–480.
- Declercq, E. R., Sakala, C., Corry, M. P., et al. (2007). “Listening to Mothers II: Report of the Second National U.S. Survey of Women’s Childbearing Experiences.” J Perinat Educ 16(4): 9–14.
- Declercq, E. R., Sakala, C., Corry, M. P., et al. (2013). “Listening to Mothers III: Pregnancy and Birth.” New York: Childbirth Connection.
- Deys, L., Wilson, V., & Meedya, S. (2021). “What are women’s experiences of immediate skin-to-skin contact at caesarean section birth? An integrative literature review.” Midwifery 101: 103063.
- Frederick, A., Fry, T., & Clowtis, L. (2020). “Intraoperative Mother and Baby Skin-to-Skin Contact during Cesarean Birth: Systematic Review.” MCN Am J Matern Child Nurs 45(5): 296–305.
- Elliott-Carter, N. and Harper, J. (2012). “Keeping mothers and newborns together after cesarean: how one hospital made the change.” Nursing for Women’s Health 16(4): 290– 295.
- Elverson, C. A., Wilson, M. E., Hertzon, M. A., et al. (2012). “Social regulation of the stress response in the transitional newborn: a pilot study.” J Pediatr Nurs 27(3): 214–224. 10.1016/j.pedn.2011.01.029
- Erlandsson, K., Dsilna, A., Fagerberg, I., et al. (2007). “Skin- to-skin care with the father after cesarean birth and its effect on newborn crying and prefeeding behavior.” Birth 34(2): 105–114.
- Ferrarello, D. and Carmichael, T. (2016). “Sudden Unexpected Postnatal Collapse of the Newborn.” Nurs Womens Health 20(3): 268–275.
- Gouchon, S., Gregori, D., Picotto, A., et al. (2010). “Skin- to-skin contact after cesarean delivery: an experimental study.” Nurs Res 59(2): 78–84.
- Gregson, S., Meadows, J., Teakle, P., et al. (2016). “Skin-to- skin contact after elective caesarean section: Investigating the effect on breastfeeding rates.” British Journal of Midwifery 24(1): 18–25.
- Hamilton, B. E., Martin, J. A., & Osterman, M. J. K. (2023). “Births: Provisional Data for 2022.” National Vital Statistics Rapid Release Report 28. Hyattsville, MD: National Center for Health Statistics.
- Henry, S., Richard-Yris, M., Tordjman, S., et al. (2009). “Neonatal handling affects durably bonding and social development.” PLoS One 4(4): e5216.
- Herlenius, E. and Kuhn, P. (2013). “Sudden Unexpected Postnatal Collapse of Newborn Infants: A Review of Cases, Definitions, Risks, and Preventive Measures.” Translational Stroke Research 4(2): 236–247.
- Hung, K. J. and Berg, O. (2011). “Early skin-to-skin after cesarean to improve breastfeeding.” MCN. The American journal of maternal child nursing 36(5): 318–324; quiz 325–316.
- Kahalon, R., Preis, H., & Benyamini, Y. (2021). “Who benefits most from skin-to-skin mother-infant contact after birth? Survey findings on skin-to-skin and birth satisfaction by mode of birth.” Midwifery 92: 102862.
- Kristoffersen, L., Bergseng H., Engesland, H., et al. (2023). “Skin-to-skin contact in the delivery room for very preterm infants: a randomized clinical trial.” BMJ Paediatr Open 7(1): e001831.
- Lanning, R. K., Oermann, M. H., Waldrop, J., et al. (2019). “Doulas in the Operating Room: An Innovative Approach to Supporting Skin-to-Skin Care During Cesarean Birth.” J Midwifery Womens Health 64(1): 112–117.
- Ludington-Hoe, S. M. and Morgan, K. (2014). “Infant assessment and reduction of sudden unexpected postnatal collapse risk during skin-to-skin contact.” Newborn & Infant Nursing Reviews (14):28–33.
- Magee, S. R., Battle, C., Morton, J., et al. (2014). “Promotion of Family-Centered Birth With Gentle Cesarean Delivery.” J Am Board Fam Med 27(5): 690–693.
- Mahlmeister, L. R. (2005). “Couplet care after cesarean delivery: creating a safe environment for mother and baby.” J Perinat Neonatal Nurs 19(3): 212–214.
- Mieso, B. R., Burrow, H., & Lam S. K. (2021). “Beyond Statistics: Uncovering the Roots of Racial Disparities in Breastfeeding.” Pediatrics 147(5): e2020037887.
- Merewood, A., Bugg, K., Burnham, L., et al. (2019). “Addressing Racial Inequities in Breastfeeding in the Southern United States.” Pediatrics 143(2): e20181897.
- Milcent, C. & Zbiri, S. (2018). “Prenatal care and socioeconomic status: effect on cesarean delivery.” Health Econ Rev 8: 7.
- Moore, E. R., Bergman, N., Anderson, G. C., et al. (2016). “Early skin-to-skin contact for mothers and their healthy newborn infants.” Cochrane Database of Systematic Reviews 11: CD003519.
- Moran-Peters, J. A., Zauderer, C. R., Goldman, S., et al. (2014). “A quality improvement project focused on women’s perceptions of skin-to-skin contact after cesarean birth.” Nurs Womens Health 18(4): 294–303.
- National Institute for Health and Care Excellence (NICE). (2022). “Intrapartum care for healthy women and babies.” . Accessed August 16, 2023.
- Nolan, A. and Lawrence, C. (2009). “A pilot study of a nursing intervention protocol to minimize maternal-infant separation after Cesarean birth.” J Obstet Gynecol Neonatal Nurs 38(4): 430–442.
- Okwandu, I. C., Anderson, M., Postlethwaite, D., et al. (2022). “Racial and Ethnic Disparities in Cesarean Delivery and Indications among Nulliparous, Term, Singleton, Vertex Women.” J Racial Ethn Health Disparities 9(4): 1161–1171.
- Phillips, R. (2013). “The Sacred Hour: Uninterrupted Skin-to-Skin Contact Immediately After Birth.” NAINR 13(2):67–72.
- Posthuma, S., Korteweg, F. J., van der Ploeg, J. M., et al. (2017). “Risks and benefits of the skin-to-skin cesarean section – a retrospective cohort study.” J Matern Fetal Neonatal Med 30(2): 159–163.
- Ray, J. G., Urquia, M. L., Berger, H., et al. (2012). “Maternal and neonatal separation and mortality associated with concurrent admissions to intensive care units.” CMAJ 184(18): E956–E962.
- Roth, L. M. & Henley, M. M. (2012). “Unequal Motherhood: Racial-Ethnic and Socioeconomic Disparities in Cesarean Sections in the United States.” Social Problems 59(2): 207–227.
- The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG). (2021). “Caesarean Section.” Accessed August 16, 2023.
- Schneider, L. W., Crenshaw, J. T., Gilder, R. E. (2017). “Influence of Immediate Skin-to-Skin Contact During Cesarean Surgery on Rate of Transfer of Newborns to NICU for Observation.” Nurs Womens Health 21(1): 28–33.
- Sakala, C., Declercq, E., Turon, J. et al. (2018). Listening to Mothers in California: A Population-Based Survey of Women’s Childbearing Experiences, Full Survey Report. Washington, D.C.: National Partnership for Women & Families.
- Sakala, C., Belanoff, C., & Declercq, E. R. (2020). “Factors Associated with Unplanned Primary Cesarean Birth: Secondary Analysis of the Listening to Mothers in California Survey.” BMC Pregnancy and Childbirth 20(1): 462.
- Schorn, M. N., Moore, E., Spetalnick, B. M., et al. (2015). “Implementing Family-Centered Cesarean Birth.” J Midwifery Womens Health 60(6): 682–690.
- Smith, J., Plaat, F., Fisk, N. M. (2008). “The natural cesarean: a woman-centred technique.” BJOG : an international journal of obstetrics and gynaecology 115(8): 1037–1042.
- Sundin, C. S. and Mazac, L. B. (2015). “Implementing Skin- to-Skin Care in the Operating Room After Cesarean Birth.” MCN Am J Matern Child Nurs 40(4): 249–255.
- Velandia, M., Uvnas-Moberg, K., Nissen, E. (2012). “Sex differences in newborn interaction with mother or father during skin-to-skin contact after Cesarean section.” Acta Paediatr 101(4): 360–367.
- World Health Organization (WHO). (2022). “WHO recommendations for care of the preterm or low birth weight infant.” Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO.
Resources:
- A video of skin-to-skin after Cesarean (https://bit.ly/3LkTj9r)
- EBB: A Doula Facilitates Skin-to-Skin in the Operating Room (https://bit.ly/3Ph8kKi)
- EBB: A Woman’s Experience with Immediate Skin to Skin after a Cesarean (https://bit.ly/3PCb0DX)
- EBB: Real Life Stories on Cesarean Care (https://bit.ly/3ZbyV07)
- NPR: The Gentle Cesarean (https://n.pr/3PzKFWY)
- Kangaroo Care March of Dimes (https://bit.ly/44MdmEr)
Acknowledgments:
We would like to acknowledge Anna Bertone, MPH, who helped update the 2017 version of this article, as well as expert reviewers from 2017: Tami Michele, DO, FACOG, OB/GYN and OB Clinical Service Chair at Spectrum Health Gerber Memorial in Michigan, and Dylan Cole, DO, FP/OB and Medical Director of Clinical Education at Moab Regional Hospital in Utah.
Birth Professionals:
Join others who also want to help bring evidence-based care to their local community.
Also, gain complimentary access to a printable library of our Signature Articles, 20+ hours of CE courses, a private community, and more.
Buy EBB Inspirational T-shirts, Due Date Buttons & Birth Affirmation Cards




Stay empowered, read more :
EBB 310 – Doulas & Nurses Advocating Together for Positive Shifts in Birth Culture with Joyce Dykema, EBB Instructor & Brianna Fields, RN
Don't miss an episode! Subscribe to our podcast and leave a review! iTunes | Spotify | YouTube Dr. Rebecca Dekker is joined by Joyce Dykema, doula and EBB Instructor, and Brianna Fields, a labor and delivery nurse, to discuss advocating for positive shifts in...
EBB 308 – The Intersection of Environmental Justice and Midwifery Care with Dr. Tanya Khemet Taiwo
Don't miss an episode! Subscribe to our podcast and leave a review! iTunes | Spotify | YouTube Curious which toxins should be most avoided for people of reproductive age and their children? In this episode, Dr. Tanya Khemet Taiwo, LM, CPM, MPH, PhD unravels the...
EBB 307 – Unexplained Infertility, Endometriosis, and a Birth Center Birth Story with Ellora La Shier, EBB Childbirth Class Graduate
Don't miss an episode! Subscribe to our podcast and leave a review! iTunes | Spotify | GoogleIn this episode, Ellora La Shier, graduate of the EBB Childbirth Class, shares about her struggle with six years of unexplained infertility and how it impacted her...